Clinical Judgement v. Checklists
Every healthcare organization has long-established programs to orient new colleagues into various roles, especially for the new graduate nurse's development and transition to practice. Transitioning from the academic study of nursing to the practice of nursing is both a tenuous time and one filled with opportunity. Shaping the course as a nurse transitions into a new role is the best opportunity to establish practice patterns that will set the individual up for a successful career and for patients to receive higher care and improved outcomes.
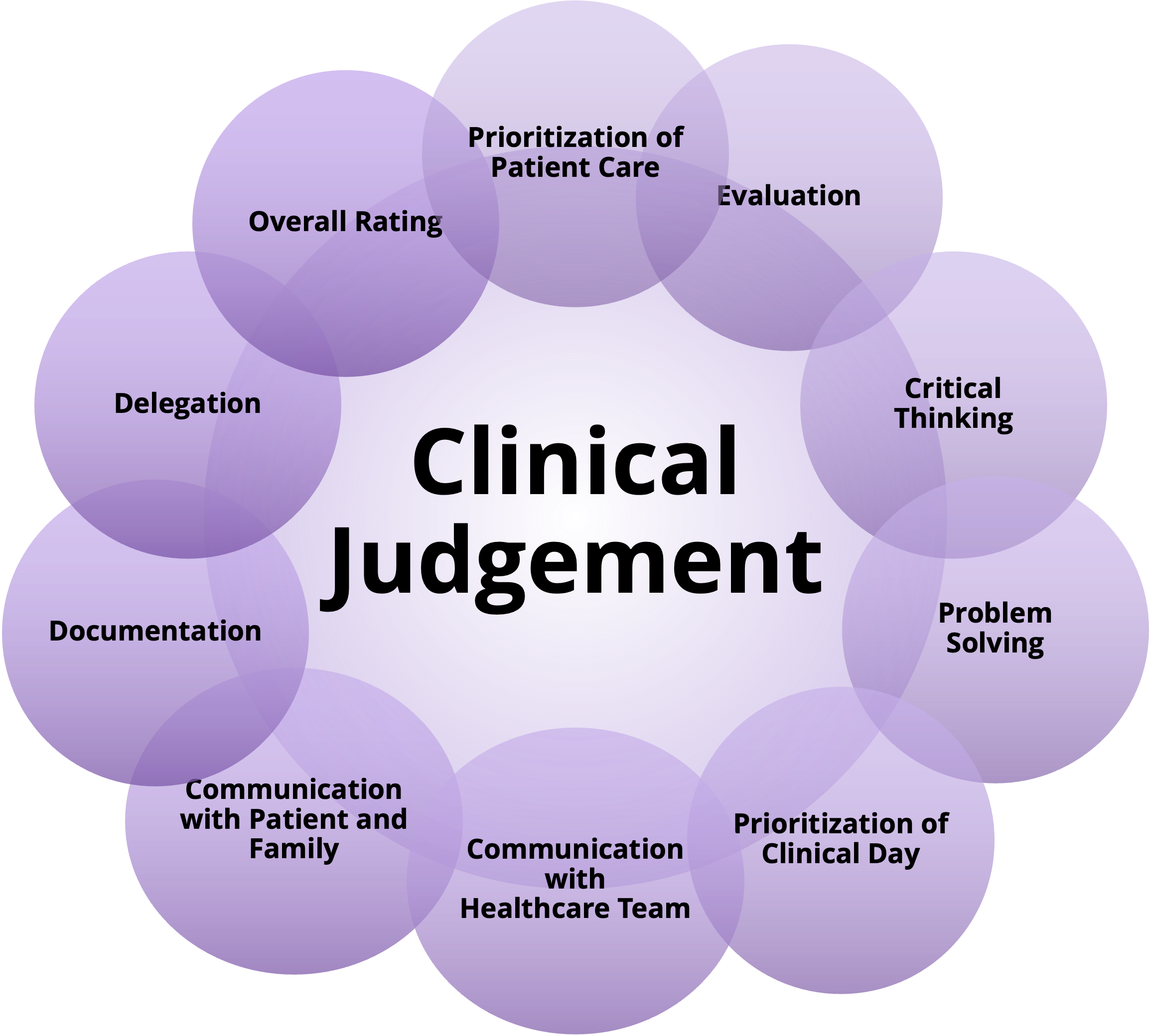 Assessing clinical judgment to determine a new nurse's readiness for independent practice is essential for ensuring patient safety and quality care. Relying solely on completing a set number of hours and experiences during orientation might not fully capture a nurse's ability to make sound clinical decisions. At the same time, exposing the new nurse to various processes and care plans is essential. A nurse must have a method to determine how to organize the care of multiple patients, select the following steps, critically think, communicate with providers, patients, and families, and delegate, document, and evaluate the effectiveness of their interventions. These professional qualities are far more critical than working through a checklist of steps and orders as they guide the nurse to prioritize, re-prioritize, collaborate, advocate, etc.
Assessing clinical judgment to determine a new nurse's readiness for independent practice is essential for ensuring patient safety and quality care. Relying solely on completing a set number of hours and experiences during orientation might not fully capture a nurse's ability to make sound clinical decisions. At the same time, exposing the new nurse to various processes and care plans is essential. A nurse must have a method to determine how to organize the care of multiple patients, select the following steps, critically think, communicate with providers, patients, and families, and delegate, document, and evaluate the effectiveness of their interventions. These professional qualities are far more critical than working through a checklist of steps and orders as they guide the nurse to prioritize, re-prioritize, collaborate, advocate, etc.
Here's how you could develop and measure clinical judgment effectively:
- Simulated Scenarios: Create realistic patient scenarios with measurable objectives and simulate them in a controlled, safe environment to assess how the new nurse approaches and manages clinical situations. This can provide insights into their critical thinking, prioritization, and decision-making skills.
- Case Studies: Present complex patient cases for analysis, where the nurse needs to assess information, identify potential problems, and propose appropriate interventions. This can demonstrate their ability to apply theoretical knowledge to real-world situations.
- Structured Reflective Practice: Encourage nurses to reflect on their experiences and decision-making processes. This can help them identify areas of improvement, develop self-awareness, and refine their clinical judgment.
- Collaboration and Communication: Evaluate how effectively the nurse collaborates with the healthcare team, communicates information, and seeks guidance when needed. Effective teamwork and communication are integral to sound clinical judgment.
- Progressive Responsibility: Gradually increase the complexity of assignments and patient care responsibilities during orientation. Monitor how the nurse adapts to these changes and makes decisions accordingly.
- Feedback from Preceptors: Experienced nurses who work closely with the new nurse during orientation can provide valuable feedback on their clinical judgment abilities, identifying strengths and areas for improvement.
- Clinical Judgment Tools: Implement validated assessment tools that measure clinical judgment skills. These tools often involve scenarios where the nurse must rank or prioritize interventions based on the patient's condition.
- Evaluate a Learner Frequently: Develop a competency assessment framework that outlines specific criteria for clinical judgment skills. Regularly evaluate the nurse's performance against these criteria throughout the orientation period. When considering frequency, trends can be identified, and progress/regression can be identified. Strengths and weaknesses will emerge, revealing opportunities for the future.
Combining these methods can provide a more comprehensive understanding of a new nurse's clinical judgment capabilities. Even in a low-frequency/high-risk situation, the new nurse will have a process they can utilize to access the resources available to them and determine the next steps. It is essential to recognize that clinical judgment involves knowledge and experience, critical thinking, prioritization, and effective communication. Using various assessment approaches, healthcare organizations can make informed decisions about a nurse's readiness for independent practice. Severing or adjusting a relationship with a nurse struggling to progress through orientation can potentially limit the impact on patient care. To the same end, supporting a struggling learner longer than usual may be an investment that returns dividends.

Topics
Popular Articles

Preceptor Rescue
Learning by doing, Learning by watching, Learning by reflecting
How can we help?
saving...